Molluscum Contagiosum
According to the Centers for Disease Control and Prevention, molluscum contagiosum is a skin infection caused by a poxvirus (molluscum contagiosum virus). The result of the infection is usually a benign, mild skin disease characterized by lesions (growths) that may appear anywhere on the body. Within 6-12 months, Molluscum contagiosum typically resolves without scarring but may take as long as 4 years.
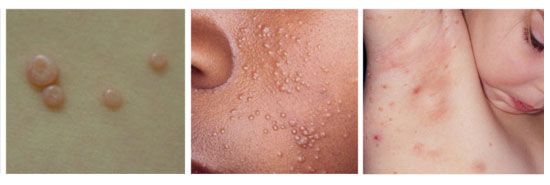
The lesions, known as Mollusca, are small, raised, and usually white, pink, or flesh-colored with a dimple or pit in the center. They often have a pearly appearance. They’re usually smooth and firm. In most people, the lesions range from about the size of a pinhead to as large as a pencil eraser (2 to 5 millimeters in diameter). They may become itchy, sore, red, and/or swollen.
Mollusca may occur anywhere on the body including the face, neck, arms, legs, abdomen, and genital area, alone or in groups. The lesions are rarely found on the palms of the hands or the soles of the feet.
What are the risk factors for molluscum contagiosum?
Anyone can get molluscum contagiosum, but certain groups of people are more likely to become infected than others. These groups include:
- children between the ages of 1 and 10
- people who live in tropical climates
- people with weakened immune systems caused by factors such as organ transplants or cancer treatments
- people who have atopic dermatitis, which is a common form of eczema that causes scaly and itchy rashes
- people who participate in contact sports, such as wrestling or football, in which bare skin-to-skin contact is common
The virus that causes molluscum spreads from direct person-to-person physical contact and through contaminated fomites. Fomites are inanimate objects that can become contaminated with virus; in the instance of molluscum contagiosum this can include linens such as clothing and towels, bathing sponges, pool equipment, and toys. Although the virus might be spread by sharing swimming pools, baths, saunas, or other wet and warm environments, this has not been proven. Researchers who have investigated this idea think it is more likely the virus is spread by sharing towels and other items around a pool or sauna than through water.
Someone with molluscum can spread it to other parts of their body by touching or scratching a lesion and then touching their body somewhere else. This is called autoinoculation. Shaving and electrolysis can also spread mollusca to other parts of the body.
Conflicting reports make it unclear whether the disease may be spread by simple contact with seemingly intact lesions or if the breaking of a lesion and the subsequent transferring of core material is necessary to spread the virus.
The molluscum contagiosum virus remains in the top layer of skin (epidermis) and does not circulate throughout the body; therefore, it cannot spread through coughing or sneezing.
Since the virus lives only in the top layer of skin, once the lesions are gone the virus is gone and you cannot spread it to others. Molluscum contagiosum is not like herpes viruses, which can remain dormant ("sleeping") in your body for long periods and then reappear.
What are the treatment options?
It is not a good idea to try and remove lesions or the fluid inside of lesions yourself. By removing lesions or lesion fluid by yourself you may unintentionally autoinoculate other parts of the body or risk spreading it to others. By scratching or scraping the skin you could cause a bacterial infection.
Physical removal
Physical removal of lesions may include cryotherapy (freezing the lesion with liquid nitrogen), curettage (the piercing of the core and scraping of caseous or cheesy material), and laser therapy. These options are rapid and require a trained health care provider, may require local anesthesia, and can result in post-procedural pain, irritation, and scarring.
However, these treatments are not popular in children as the physical removal of the lesions can be painful and burn the skin.
Topical Preparations

Scientific Case Study:
A 4-year-old child was diagnosed with a skin viral infection by molluscum contagiosum, which had a moderate effect (40% impairment) on the child’s quality of life. The caregivers were recommended a compounded medicine. Following 2 weeks of treatment, the condition was resolved and there was no impairment on the child’s quality of life.
A commonly requested compounded medication for patients that have molluscum contagiosum is a topical cream with cimetidine, deoxy-d-glucose, EGCg, ibuprofen, and tea tree oil.
This testimonial came from a mother who had the opportunity to use a compound for molluscum on her daughter and had a very positive experience:
“My daughter presented molluscum on her entire neck when she was seven years old. In addition to being really itchy and often painful, she was embarrassed with how it looked in such a visible area. We took her to the pediatrician who said that it could take 8-18 months to completely heal. After using the compounded preparation, my daughter’s lesions cleared within four weeks."
Prevention
How can I keep it from spreading?
The best way to avoid getting molluscum is by following good hygiene habits. Remember that the virus lives only in the skin and once the lesions are gone, the virus is gone and you cannot spread the virus to others.
Wash your hands
There are ways to prevent the spread of molluscum contagiosum. The best way is to follow good hygiene (cleanliness) habits. Keeping your hands clean is the best way to avoid molluscum infection, as well as many other infections. Hand washing removes germs that may have been picked up from other people or from surfaces that have germs on them. See the Handwashing site for more information.
Don’t scratch or pick at molluscum lesions
It is important not to touch, pick, or scratch skin that has lesions, that includes not only your own skin but anyone else’s. Picking and scratching can spread the virus to other parts of the body and makes it easier to spread the disease to other people too.
Here's an example of two types of watertight bandages you can find in your local drugstore. Image courtesy Edie Lederman, MD, CDC.
Keep molluscum lesions covered
It is important to keep the area with molluscum lesions clean and covered with clothing or a bandage so that others do not touch the lesions and become infected. Do remember to keep the affected skin clean and dry.
Any time there is no risk of others coming into contact with your skin, such as at night when you sleep, uncover the lesions to help keep your skin healthy.
Be careful during sports activities
Do not share towels, clothing, or other personal items.
People with molluscum should not take part in contact sports like wrestling, basketball, and football unless all lesions can be covered by clothing or bandages.
Activities that use shared gear like helmets, baseball gloves and balls should also be avoided unless all lesions can be covered.
Swimming should also be avoided unless all lesions can be covered by watertight bandages. Personal items such as towels, goggles, and swim suits should not be shared. Other items and equipment such as kick boards and water toys should be used only when all lesions are covered by clothing or watertight bandages.
Other ways to avoid sharing your infection
Do not shave or have electrolysis on areas with lesions.
Don’t share personal items such as unwashed clothes, hair brushes, wrist watches, and bar soap with others.
References
1. KidsHealth® (no date) Infections: Molluscum Contagiosum. Available at: http://kidshealth.org/en/parents/molluscum-contagiosum.html# (Accessed: 29 June 2018).
2. Centers for Disease Control and Prevention (2015) Molluscum Contagiosum. Available at: http://www.cdc.gov/poxvirus/molluscum-contagiosum/ (Accessed: 29 June 2018).
3. American Academy of Dermatology (2015) Molluscum Contagiosum. Available at: https://www.aad.org/dermatology-a-to-z/diseases-and-treatments/m---p/molluscum-contagiosum (Accessed: 29 June 2018)
